Simultaneous Implant placement with bone augmentation using GBR technique By Dr. Teoh Chang I Chun
- Yu Wicky
- Nov 7, 2022
- 5 min read
Dental implants have well been established as a predictable treatment option for restoring partially edentulous cases (Pjetursson el al 2012). It is recommended to have adequate dimension of bone volume for optimal three-dimensional implant placement (Resnik and Misch 2017). For a stable and predictable outcome, it was suggested 2mm or more of bone width around the implant, especially buccally at the crestal area of the alveolar ridge, for long-term bone stability (Spray et al 2000, Grunder et al 2005). Often, clinicians may face situations whereby the width of the alveolar ridge is less than optimal width, then there is a need to increase the ridge width to 6 to 8mm either prior to or simultaneously with implant placement. Guided bone regeneration (G.B.R.) is one of the most deployed techniques for such purpose (Buser et al 1996). Although a few authors had demonstrated the effectiveness of using biomaterials such as ABBM protected with resorbable collagen membrane (Hammerle et al 2008). However, there is concerns of graft displacement at the ridge crest caused by the pressure of closing the overlying flap (Urban 2017).
This article is a case report on simultaneous implant placement together with Guided Bone Regeneration.
Case Report
-
A 60-year-old gentleman with no relevant medical history requested for implant treatment in Q4. He recently lost 47 and presented with Free End Saddle in the lower right mandible. Clinical examination, Panoramic radiograph, and Cone Beam CT scan (Fig 1, 2 & 3) indicated the lower right alveolar ridge of sufficient dimension of was available for implant placement. The final treatment plan was to place two implants in 45 & 46 region with simultaneous bone augmentation using Guided Bone Regeneration. The treatment plan and procedure were carefully explained to the patient and a consent document was signed by the patient to signify the agreement of treatment.
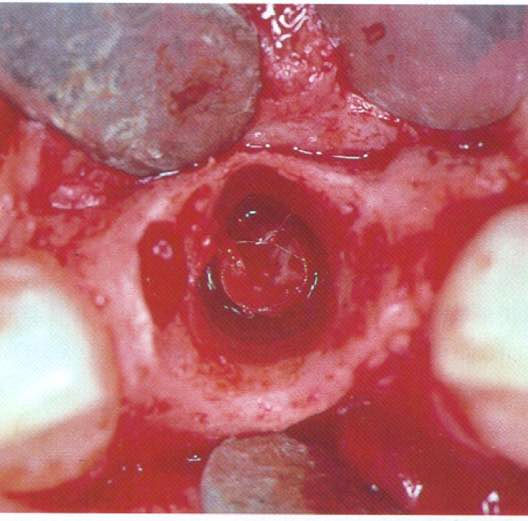
Local anaesthesia (Xylestein A 3M ESPE) was given with buccal and lingual infiltration, and Inferior Dental block was avoided. The surgery started with a mid-crestal incision plus intrasulcular incision around buccal of 44 and ending up with mesial releasing incision at 44, which would allow better access to buccal side of the alveolar ridge. A full thickness mucoperiosteal flap was then elevated on both buccal and lingual side. It is important to identify the surgical landmark such as the mental foramen on the buccal side, where the mental nerve emerged, the mylohyoid muscle on the lingual side. The alveolar ridge was completely exposed. Any remnant of soft tissue on the bone surface should be removed (fig 4). The width of the ridge crest was around 5mm and there was good bone height (> 14mm) above the Inferior Dental Canal. Implant osteotomy site preparation was carried out following the protocol described by the manufacturer (NeoDent). The osteotomy site preparation at 45 received special attention in order to avoid damaging the Mental Nerve (Fig 8, 9). 2 x NeoDent 3.7mmD x 10mmL and 4.3mmD x 10mmL were inserted with good primary stability (60Ncm torque) (Fig 5, 6, 7 & 10). The implant heads were placed so that they were levelled with the crestal bone. Although the implants were cover with bone, minor dehiscence area presented on buccal and lingual sides. Autogenous bone was harvested with bone collector (NeoBiotec ACM) using straight handpiece at slow speed (150 RPM) Fig 11, 12. The bone chips harvested were then mixed with ABBM (Bio-Oss) particles to increase its volume and stability. The bone graft mixture was then placed on buccal and lingual side of the implants and protected with a collagen membrane (OssGuideÒ) which was in turn stabilized with bone tacks (Ustomed). The bone tacks helped to keep the membrane in position and prevent migration of the bone graft materials. Periosteal releasing incision was made on the buccal flap, the objective is to elongate the buccal flap to provide a tension free primary closure. Buccal and lingual everted flap margins were secured with multiple sutures.
Fig 1. Pre-treatment Panoramic radiograph.

Fig 2. Cross section scan in.

Fig 3. CBCT scan revealed the ridge dimension was narrow in 45 & 46 area.

Fig 4. Exposure of the entire alveolar ridge including the mental foramen and mental nerve.

Fig 5. Insertion of NeoDent 4.3mmD x 10mmL implant in 46 site.

Fig 6. Rachet tool was used to insert the implant to its final position.

Fig 7. Good primary stability (60Ncm torque) was achieved.

Fig 8. Mental foramen was identified, and mesial extension was measured with a periodontal probe.

Fig 9. Implant osteotomy site was well above the Mental foramen.

Fig 10. Two NeoDent implants were inserted with good primary stability.

Fig 11. Donor site in retromolar area.

Fig 12. Autogenous bone chips harvested with Bone collector

Fig 13. Xenograft (Bio-Oss particles) was mixed with autogenous bone chips.

Fig 14. Collagen membrane was initially placed on the lingual side.

Fig 15. The collagen membrane was stabilised with bone tacks on lingual side.

Fig 16. Graft mixture was placed on buccal and lingual side of the alveolar ridge.

Fig 17. Bone tacks on buccal side to stabilise the collagen membrane.

Fig 18. Buccal periosteal releasing incision was made for flap elongation.

Fig 19. Tension free flap closure was achieved.

Fig 20. Post treatment Panoramic radiograph.

Conclusion
High insertion torque values can be achieved when dental implants are placed completely within the native bone. However, when the remaining bony wall is thin on either buccal or lingual side, it is recommended to increase the hard tissue thickness with bone augmentation procedure. GBR is a highly successful and predictable technique. Inclusion of autogenous bone particles will enhance bone formation next to alveolar ridge. It is also important to stabilize the collagen membrane with bone tacks or fixation screw to prevent unwanted movement of the bone graft materials under the pressure of closing the soft tissue flap (Mari et al 2016). This paper highlighted such an approach with implant placement and simultaneous bone augmentation with GBR technique.
Reference
Pjetursson BE, Thoma DS, Jung RE, Zwahlen M. A systematic review of the survival and complication rate of implant-supported fixed dental prstheses (FDPS) after a mean observation period of at least 5 years. Clin Oral Implants Res 2012;23(Suppl 6):22-38.
Resnik RR, Misch CE. Misch’s avoiding complications in Oral Implantology. Elsevier, St. Louis, Missouri 234-266.
Spray JR, Black CG, Morris HF, Ochi S. The influence bone thickness on facial marginal bone response: Stage 1 placement through stage 2 uncovering. Ann Periodontol 2000:5(1):119-128.
Grunder U, Gracis S, Capelli M. The influence of the 3 D bone to implant relationship on aesthetics. Int J Period & Rest Dent 2005;25(2):113-119.
Buser D, Dula K, Hirt HP, Schenk RK. Lateral ridge augmentation using autografts and barrier membranes: a clinical study with 40 partially edentulous patients. J Oral Maxillofac Surg 1996;54:420-432.
Hammerle CH, Jung RE, Yaman D, Lang NP. Ridge augmentation by applying bioresorbable membranes and deproteinized bovine bone mineral: a report of twelve consecutive cases. Clin Oral Implants Res 2008;19:19-25.
Urban I. Vertical and Horizontal ridge augmentation: New perspectives. 2017 Quintessence Publishing Co. Ltd. Surrey, UK Ch 11;117-145.
Mari J, Wui H, Jung RE, Hammerle CH, Benic G. Influence of blinded wound closure on the volume stability of different GBR materials: an in vitro cone-beam computed tomographic examination. 2016;27(2):258-265.




Comments